Imagine you’re thirty-eight years old, a parent with two kids, and you get diagnosed with cancer. Let’s take it one step further to say it’s pancreatic cancer.
That’s the not-so-good news.
The good news is: as you’re learning of your cancer, you soon come to find that your wife is a few weeks pregnant. Now you plan to be a parent of three kids—so congratulations are in order.
This, in fact, is the case for my cousin as we speak. He’s like my brother.
Now here’s what I’ve been able to learn about precision medicine and cancer from:
- working with a private equity client—they’re a precision medicine healthcare fund; and
- researching top institutions and world-renowned surgeons in the wake of my cousins diagnosis.
Bottom line: you must align yourself with a capable general contractor to help ‘data mine’ and organize all the conflicting information so you can cross the finish line.
Easier said than done.
Naturally, the first and last resort for most cancer patients is to abide by the well-intentioned advice of the doctor. Especially, if that doctor is stationed at a world-renowned cancer center.
But here’s the hidden problem I found with that method:
- 99% of top cancer institutions—the big names in the USA—currently use genomic tests to scan the cancer.
- For the most part, they completely ignore proteomics.
Repeat: as far as the standard operating procedure for most of the big cancer centers in the USA, they are only testing genomics so to get to know the tumor.
That’s like going to fight a war and someone tears the battle map in-half so that the army general can only see ½ of the map.
How can one expect to fight a war when ½ the battlefield is unknown?
Here’s reality: Most lab testing companies offer a pre-specified panel of genomic evaluation—a panel of specific DNA and RNA genes and transcripts to see if the patient’s tumor has abnormalities.
They do not measure proteins.
Yet, it’s proteins that control the cell.
Therefore, cancer institutions which use labs that only run genomics tests don’t base the treatment options on proteins or other multi-omic information.
That’s problem one.
This then leads us to problem two: Which is to match the right drug to the right cancer.
(what’s called Precision Medicine)
All the big institutions claim to be using Precision Medicine.
But as we just mentioned, how precise can you be if you only scan 1/2 the battle-field?
In a moment, I’ll share with you a contractor that you might choose to add to your A-Team. A contractor that aggregates lab data from genomics, proteomics and more.
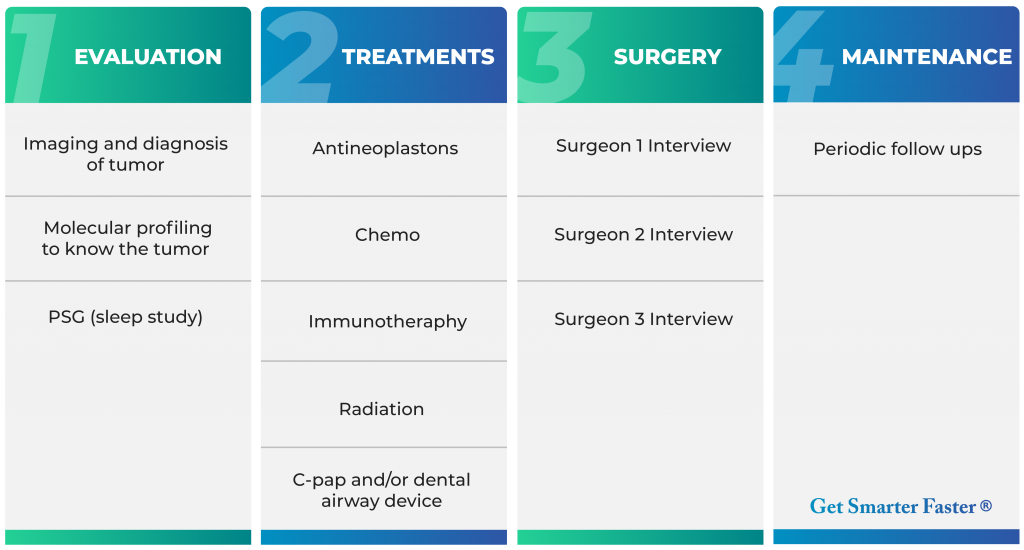
But first, let me show you a 4-phase process that I would use to manage my own cure… if I had cancer.
(This isn’t medical advice; you have a physician for that. This is an HK Peak Performance flow)
With cancer, you don’t have the luxury of time. Especially, pancreatic cancer. So you need a process to reduce delays and manage the patient’s A-Team of contractors.
Here’s a simple four phase process to manage a cancer battle plan.
This is what I would do if it were me.
In Phase 1, it would seem the ultimate goal is to get confirmation that it’s cancer. Furthermore, this is where the proper molecular profiling of the tumor can take place: To know the tumor. For molecular profiling, if it were me, I would get more than just genomics.
I would get all “omic” tests—especially proteomics. If it were me, I would get a sleep apnea test to document any apnea. Because if I’m suffocating or experiencing resisted airflow in my sleep due to sleep apnea, then I know treating the sleep apnea will help my body, brain, heart, fatigue and full body performance. It’s estimated that 80% of the cases of moderate and severe obstructive sleep apnea in the United States are undiagnosed. Big problem.
(to avoid delays with sleep testing, simply make a dental device from day one).
In Phase 2, a creative doctor will be able to prescribe the proper treatments because the entire battle-field will have been scanned. And if suffocating during sleep—even with mild apnea—to take steps and properly stabilize the airway with C-pap and/or a dental device which will offer huge health advantages in achieving peak performance.
In Phase 3, is for surgery—if it’s even necessary. It’s possible for Phase 2 treatments to cure the cancer. Maybe no surgery needed. But if it was me, I would find two or three top surgeons in the earlier phases. To Know Your Personnel.
Hopefully, the surgeon won’t be needed.
Nevertheless, I would interview the top surgeons for my specific cancer in advance. To know my A-Team of contractors. Know Your Personnel.
Phase 4, maintenance: is the follow-up hygiene that might be required after beating cancer. Just like going to see the dentist to check your teeth periodically, the oncologist might wish to see the patient periodically. No problem.
For a cancer patient, phase four means victory.
Molecular Profiling Cancer
Now, as far as getting to know the tumor with molecular profiling, here’s who I would consider if I had cancer. As of this writing, I would consider Perthera, Inc. for molecular profiling of the tumor biopsy.
Perthera is not a lab per se.
Perthera is an aggregator of lab data.
They work with the top genomics and proteomics labs, among others. They will accept the patient’s biopsy and the information from the lab companies. Then Perthera will take the lab results from the genomics lab contractor. They will also take the protein data from the proteomics lab, along with any previous treatment history.
All this data then gets dumped into Perthera’s Therapeutic Intelligence Engine.
The machine then aggregates this data across ~ 50,000 rules to come up with a ranked therapy list of options for the patient—individualized to the specific patient based on all this data.
In a nutshell, the Perthera scan can be a key part to the doctor’s treatment decision because it allows the physician to have the most comprehensive analysis while offering extensively ranked therapies.
This four phase process is how I would package my A-Team to beat cancer.
And God is the glue.
P.S. As of this writing, Perthera has no cost to the patient for their service. However, expect the proteomics lab scan of the biopsy to run about $6,000; and the genomics lab scan to cost the same amount.
Therefore, expect roughly $12K-$13K for the lab tests. With the majority of lab costs typically covered by the patient’s insurance. Then Perthera will aggregate the data and run a report at no cost. A full-report of ranked options will be given to the A-Team.
P.P.S. This is not medical advice; you have a physician for that.